 In the alphabet soup of healthcare, often the initial drivers of large-scale initiatives are government reporting and regulatory requirements, like All Payer Claims Databases (APCD) and Health Information Exchanges (HIE). These requirements encourage interoperability and data sharing between stakeholders.
In the alphabet soup of healthcare, often the initial drivers of large-scale initiatives are government reporting and regulatory requirements, like All Payer Claims Databases (APCD) and Health Information Exchanges (HIE). These requirements encourage interoperability and data sharing between stakeholders.
These efforts aren’t new or news – but the past decade has focused on identifying assets, bringing the data in, and analytics that match patients across sources.
Government agencies at all levels (both in the U.S. and abroad) are moving into the next phase of this journey. They are going beyond data access and blending and focusing on using the data strategically to improve care and lower costs.
Registries Power Population Health Programs
When faced with a large population data set, it can be a challenge to target a single focus area that has both meaning and impact. Clinical data registries are a perfect example of macro-level data used for micro-level initiatives. When these targeted initiatives achieve measurable results, this leads to tremendous power for population health initiatives.
We’ve seen the role registries play in quality improvement successes at specialty-focused organizations. They’ve driven important and renowned innovations in care delivery. This has been accomplished through the symbiotic relationship between a culture of engaged physicians and the use of trusted data and powerful technology. The technology allows for a window into physician performance and patient outcomes.
When planning how to make a patient registry part of your population health program, there are two parts to consider:
- Registry Technology
- Registry Strategy
Part 1: Technology of Building a Clinical Data Registry for Population Health
A clinical data registry is built on the ingestion of real-world data and the transformation of that data through advanced analytics into actionable real-world evidence. Let’s break this process down into 3 key steps.
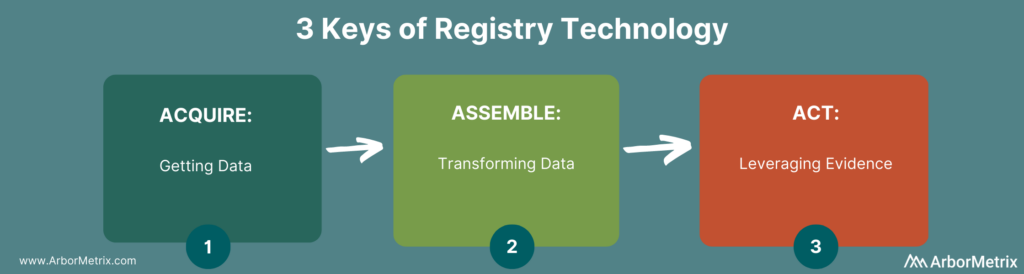
- Data Acquisition: Acquisition can include a broad spectrum of options. One option is machine-to-machine connections to EHRs, government assets, and other databases. There are also human-to-machine connections as needed for data entry from providers and patients. This includes more granular disease-specific elements and longitudinal outcomes outside of routine care visits.
- Data Assembly: Assembly can include validation and cleansing for quality, and transformation for analytic purposes. This includes creation of clinically specific measures, risk adjustment for fair case mix comparisons, patient matching, benchmark creation, predictive models, and more. This transformation is key to building trust in the data.
- Acting on Evidence: Leveraging evidence is facilitated by our intuitive and user-friendly AMxCore product that provides visibility into all individual data elements attributed to patients, as well as aggregate reporting that provides deep insights into trends, patterns, and opportunities for change.
In large initiatives, so much time is spent on acquiring data that transforming it and utilizing it effectively are afterthoughts. While data is foundational and fundamental, a strong strategy behind the technology ensures a speed to value and long-term registry success.
Part 2: Strategy of Building a Clinical Data Registry for Population Health
A registry toolset needs to go beyond technology and data access and produce information of such quality that it can be relied upon to improve the standard of care across entire health systems, states, or countries.
At its strategic core, a registry is a very simple concept broken into 3 parts.
 Curated Data Elements
Curated Data Elements
The curated data elements are considered and selected from the broad set of data assets available and used to create a defined Data Dictionary. While in some cases, gathering as many data elements as available has value (often the foundation of initiatives like HIEs and APCDs), most successful quality improvement initiatives only utilize a subset of these elements. Strategically curating these assets ensures the most relevant and meaningful elements are being collected, validated, and transformed for purpose-driven use in the context of specific diseases or conditions.
Measurement Strategy
The measurement strategy transforms data into information through the rigorous application of data science principles. These principles create trusted data assets that can quantify outcomes and identify the drivers of those outcomes. This trusted data gives, agencies, hospitals, or physicians the resources they need to better understand and improve care. This is the strategic heart of a registry – data that is trusted to enact important care delivery changes.
Targeted Focus
A targeted focus is the identification of high-priority questions your agency or organization needs to answer about the providers, patients, and processes under your influence. Starting with a focus ensures that you are pointed at achievable opportunities for change.
Think: reduce surgical site infection rates, not reduce mortality. This focus ensures that you are targeting true opportunity for improvement that will be measurable and repeatable across the system of care.
Operationalize Large Scale Quality Improvement
When you apply this strategic framework on top of strong registry technology, you can operationalize and catalyze large scale improvements in care delivery – across organizations, agencies, and around the world. To learn more about how to evaluate your registry technology, check out my post: 3 Technology Essentials for Patient Registries that Improve Care.
