What Is Predictive Analytics and Why Is It Important?

Exploring data helps us understand our world. Why something happened, how things are trending, and what constitutes a meaningful change.
Now, we have a vast set of tools in our data analysis toolbox. We can not only examine what happened in the past, but we can also predict what might happen in the future using predictive analytics.
Predictive analytics is a powerful tool that can help us accelerate the path to healthcare value, ultimately reducing healthcare costs while improving patient care.
Read on for an introduction to predictive analytics in healthcare, including the uses, benefits, value, and potential future of predictive analytics.
In this post we will cover:
- What Is Predictive Analytics in Healthcare?
- What Is the Role of Predictive Analytics?
- What Are Use Cases of Predictive Analytics in Healthcare?
- What Is the Value of Predictive Analytics?
- What Is the Future of Predictive Analytics?
What Is Predictive Analytics in Healthcare?
Predictive analytics answers the question: what is likely to happen next?
Using modeling and forecasting techniques, predictive analytics helps determine what has a high probability of occurring in the future. Physicians, researchers, medical specialty societies, pharmaceutical companies, and every other healthcare stakeholder can then use those predictions to provide the best possible care for individual patients.
To provide the most robust predictions possible, predictive analytics uses a variety of modeling techniques, from traditional hierarchical linear models to advanced artificial intelligence (AI) and machine learning algorithms. AI is a collection of technologies that can think and adapt on their own, while machine learning, which is a subset of AI, involves generating models to describe data with greater and greater precision as more data is introduced. [1,2]
In healthcare, predictive analytics leverages AI and machine learning to analyze historical data and forecast outputs such as disease risk for individual patients. [3]
What Is the Role of Predictive Analytics?
Predictive analytics is quickly becoming a cornerstone of personalized healthcare.
Using AI and machine learning, predictive models can intake huge amounts of diverse data for a single patient and forecast a patient’s response to certain treatments or devices, their risk of developing a specific disease, and their prognosis for a given condition.
What is personalized healthcare? This customized way of treating a patient is rooted in that individual’s specific medical history, environment, social risk factors, genetics, and unique biochemistry, among other characteristics. The key to personalized healthcare is treating a patient based on their specific attributes, instead of relying on population averages that aren’t one-size-fits-all. [4]
Predictive analytics is helping the healthcare system shift from treating a patient as an average to treating a patient as an individual, which can only improve patient care overall in terms of quality, efficiency, cost, and patient satisfaction.
Use Cases of Predictive Analytics in Healthcare
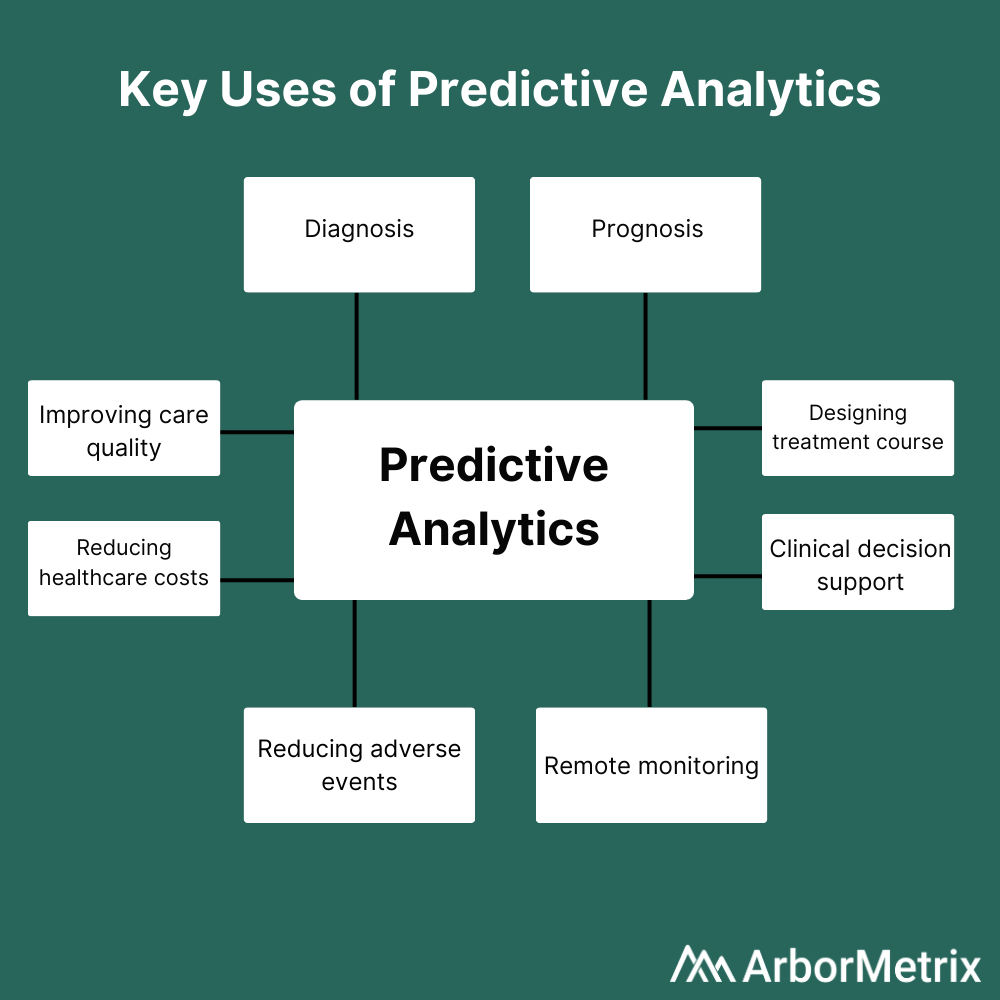
Predictive analytics is useful at every step in a patient’s journey, including diagnosis, prognosis, and treatment. Predictive analytics can also inform remote patient monitoring and reduce adverse events. On a more macro level, predictive analytics can improve care quality while reducing costs.
 Leveraging predictive analytics can help answer questions like:
Leveraging predictive analytics can help answer questions like:
- What is the best course of treatment for this patient?
- Is this patient likely to experience an adverse event following a given procedure?
- What is the likelihood that this patient has a malignant tumor?
Here are a few key examples of predictive analytics in healthcare being used at various points in the patient journey:
- Diagnosis: Predictive analytics have been used to predict malignant mesothelioma diagnoses in a patient cohort. Patients diagnosed early can start treatment immediately, which improves their chances of survival—thus making prediction a critical tool. [5]
- Prognosis: Researchers used predictive analytics on physiological data from patients with congestive heart failure (CHF) to predict which patients were at greatest risk of readmission following a hospital stay. Using that information, physicians could implement interventions early to prevent the predicted readmissions. [6]
- Treatment: Clinicians have used machine learning-based predictive analytic models to determine the most effective course of treatment for chronic pain patients. [7]
Most importantly, predictive analytics can provide real-time clinical decision support at the point of care, making personalized healthcare as efficient as possible.
This is just a small sliver of the research being performed using predictive analytics in healthcare. As technology and analytic models advance, more opportunities to improve patient care using forecasting techniques will surely be discovered.
What Is the Value of Predictive Analytics?
Wherever there is data, predictive analytics can produce tremendous value. Leading organizations leverage predictive analytics to generate real-world results. Let’s look at an example below.
Michigan Bariatric Surgery Collaborative (MBSC) Uses a Predictive Calculator to Forecast Bariatric Surgery Outcomes
MBSC, a quality improvement collaborative funded by Blue Cross Blue Shield, leverages a powerful patient registry to improve bariatric surgery in Michigan.
MBSC uses clinical and patient-reported data combined with powerful predictive analytics to support clinical decision-making. Participating physicians use the MBSC registry and patient engagement tools to collect comprehensive preoperative data for potential bariatric surgery patients.
This data is then used to feed the MBSC Predictive Outcomes Calculator, a publicly available tool physicians can use to predict a patient’s weight loss, comorbidity resolution, and complication rate after bariatric surgery.
Specifically, the tool uses patient information on demographics, comorbidities, and other risk factors to forecast:
- Predicts weight loss at years 1, 2, and 3 for each of the available procedures.
- Predicts the likelihood of resolving weight-related comorbidities such as diabetes or sleep apnea.
- Predicts the likelihood of adverse events, serious complications and mortality.
Notably, the predicted rates for weight loss, comorbidity resolution, and potential complications are patient-specific, using risk-adjusted, real-world outcomes data from similar patients. These tools and other quality improvement initiatives helped MBSC and its members decrease rates of venous thromboembolism (VTE) by 43% and decrease post-surgical death rates by 67%.
What Is the Future of Predictive Analytics?
As we amass more and more data, predictive analytics will become both more common and more accurate.
Currently, many predictive models use traditional statistical methods, such as logistic regression, which are useful and can provide insightful results. However, AI and machine learning methods such as random forests, when implemented appropriately, can provide more accurate predictions. Ultimately, as more feature-rich data is collected and as the collection process itself improves, predictive analytics can take advantage of deep learning algorithms that can make better use of large and complex data sets. [8]
For example, deep learning algorithms can be used for image recognition, whether that be images gleaned from MRIs or other types of imaging technology, to automatically detect certain features. In contrast, a machine learning-based approach would require the radiologist to extract all the features from the image first. Deep learning simplifies the process by detecting all the features automatically, without requiring extra work by the radiologist.
Put simply, big data and predictive analytics in healthcare go hand in hand—more data means better predictions.
Additionally, the field of predictive analytics will advance to overcome its limitations. One current drawback is that predictive analytics is not able to provide insight into what might happen after an intervention or other change, which can be frustrating for researchers and clinicians who want to understand how patients might fare after a new treatment or as a result of a new hospital procedure. We expect predictive analytics will advance past this challenge, allowing researchers to forecast the future in a much more expansive and holistic way.
Predictive analytics will also be able to benefit from the massive leaps in computer processing power that make chewing through complicated algorithms possible.
Someday soon, predicting the future with accuracy under a variety of conditions will be the norm, not a fortune-teller’s trick.
Whichever Direction Your Predictive Analytics Journey Takes You, You’ll Need a Guide
The Top 3 Lessons for Registries from the CMSS Annual Meeting

The Council of Medical Specialty Societies (CMSS) held their 2020 Virtual Annual Meeting with the theme of Covid-19 and Beyond: Digital Transformation of Healthcare, Research, and Education.
The dynamic group of presenters and panelists covered a variety of topics that demonstrate how digital technology, such as clinical registries and healthcare analytics, can be instrumental in advancing healthcare.
Our key takeaway: The digital transformations that are needed to make these advancements are less about how people transform technology and more about how technology transforms people and lives.
Registries, for instance, can be used to help solve some of the most intractable issues in healthcare like:
- Addressing underlying root causes of health disparities.
- Making it easier for patients to understand, navigate, and manage their care.
- Monitoring and managing COVID-19 and other emerging priorities.
1. Addressing Root Causes of Health Disparities
There are widespread and longstanding health disparities among racial and ethnic minorities.
These disparities cause some populations to face unfair health burdens. Health is a fundamental human right, and consequently, healthcare stakeholders have an ethical obligation to ensure fair and just health experiences by acting to eliminate avoidable health disparities.
Clinical data registries are powerful tools for assessing health disparities, identifying the root causes, and tracking efforts to address health inequities. Importantly, these tools should provide actionable insight, as referenced by Rhea Boyd, M.D., M.P.H., Pediatrician and Child Health Advocate at Palo Alto Medical Foundation and UCSF Benioff Children’s Hospital.
This work includes implementing robust data logic rules to identify underperformance in need of equity-focused quality improvement efforts, as presented by Ernest Moy, M.D., M.P.H., Executive Director, Office of Health Equity, U.S. Department of Veterans Affairs. Those health equity efforts are made more effective with social determinants of health analytics that provide a comprehensive view of the interconnected factors influencing a patient’s health.
How Registries Can Advance Health Equity
Alongside several of our partners at medical specialty societies, we see the very real effects of longstanding and systemic health disparities – made evident through evaluating data in their registries.
Registries collect a high-volume of data from different sources and deliver high-quality, data-driven insights. Efforts to reduce health disparities require data to detect and measure the impact of disparities, identify the complex and interconnected determinants, and inform interventions and best practices.
Efforts to advance health equity through registries fall into three activities:
- Measuring health disparities. To reduce health inequities, we need methods to measure disparate health outcomes and methods to assess the impact of those disparities across different types of health indicators.
- Assessing underlying factors. Effectively addressing health disparities requires understanding the underlying factors influencing disparate outcomes.
- Forming and evaluating interventions. By assessing health disparities and their underlying factors, we will have insights to develop impactful interventions and sustaining widespread health equity improvements through tracking best practices.
2. Helping Patients Understand Their Care and Outcomes
Healthcare is complex. Patients can be overwhelmed as they try to understand, navigate, and make important decisions about their care.
Consider a patient with a chronic condition who might have up to 20 healthcare providers, all generating assessments and treatment plans that must be coordinated and aligned. Even people who have spent their life working in healthcare can feel overburdened by the amount and complexity of information presented to patients.
More patients are now turning to technology to help them through their care journey. And now more technology is becoming patient-centric to help patients overcome common barriers they face in their healthcare.
For example, registries can offer patient engagement tools that provide patients with meaningful support as they interact with their health. Registry patient portals should offer key types of support to improve patient experiences and health outcomes:
- Instrumental Support. Tangible services and functions, such as capabilities to directly connect to their care team or participate in clinical trials or research.
- Informational Support. Connection to tailored patient resources that provide advice, suggestions, and clinical insights.
- Appraisal. Personalized registry data can be presented back to patients in easy-to-review graphs. This can show patients how they are progressing throughout their treatment, which helps patients to self-evaluate their progress and health experiences.
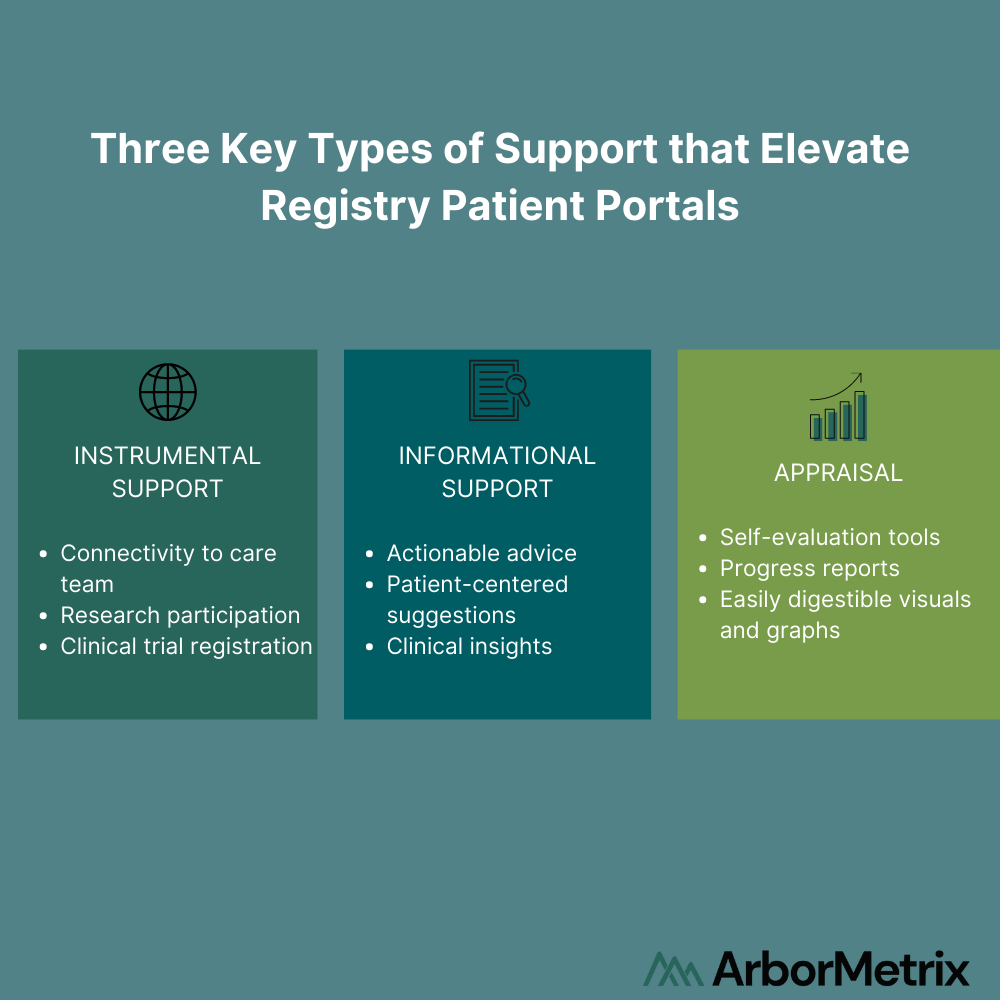
As described by Donna Cryer, JD, President and CEO of the Global Liver Institute, these patient-centric technologies give patients supportive communities and influential tools to elevate a patient’s voice and help them maximize their health.
3. Understanding a Global Pandemic
Monitoring, managing, and understanding COVID-19 was top-of-mind throughout several sessions. Registries are playing a central role in this.
Modern registries can address emerging health issues like the pandemic with rapid measurement and quick discoveries.
There are three key parts to doing this successfully:
- Determining the priorities and research questions a registry can uniquely answer.
- Using trusted data and advanced analytics to address critical issues.
- Leveraging a flexible data infrastructure to pivot at any time – modern clinical data registries are designed to evolve.
Several organizations are already leveraging their registries and data infrastructure to be proactive in measuring, monitoring, and addressing the COVID-19 pandemic. You can learn from them and find more strategies in our blog post “Best Practices for Clinical Registries with New Research Priorities.”
Registry Technology Should be People-Centric
Overall, digital transformations are about using technology to solve issues for people, not simply about using people to solve technology issues.
It is less about being technology-centric than it is about making technology people-centric. Registries are powerful tools that can be designed to address some of the most widespread health issues affecting people, while also engaging patients in innovative ways to improve their health experiences.
From defining the vision for a registry program to designing surveys and reports for clinicians and patients, we take a person-driven approach.


